We may feel weary of Covid 19, but the virus continues to evolve and our immunity autumn booster vaccine is offering vaccines to those they consider at highest risk from a Covid 19 infection, including people who are pregnant, with certain underlying medical conditions, and those aged over 65.
The autumn booster shots on offer in the UK are a mixture of vaccines including the previously used bivalent vaccines, (that target the original strain of SARS-CoV-2 (the virus that causes COVID-19) alongside an omicron variant) and mRNA vaccines that target XBB1.5.
Why do we need boosters?
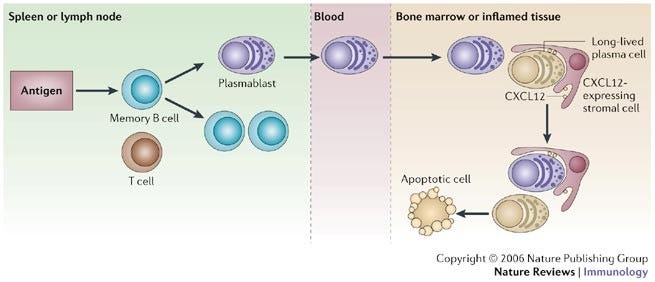
There are two main reasons for needing boosters. One is that our immunity wanes. Most of the current crops of vaccines prompt white blood cells called B plasma cells to start making antibodies specific to the virus. We can readily measure those antibodies in our blood. Over time these antibody making factories die out as they are not very long lived cells- meaning that the levels of antibody circulating in our blood falls to very low levels. There is just not enough antibody to protect against getting a re-infection. However, we may still have low levels of circulating antibody which is topped up by special cells in our bone marrow that are more long lived- long-lived plasma cells. Memory cells are another important immune cell- specialised long-lived immune cells that remember the virus and carry instructions for B cells to be quickly deployed if it attacks again. Downside of all this is that whilst your immune system gears up to make more antibody, you can get sick again.
Immune evasion
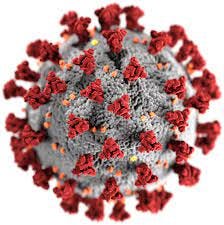
The other reason we need new vaccines is that SARS-Cov-2 just keeps changing and this REALLY matters. Most vaccine candidates in use target the spike structures- that the spiky bits on the schematic below. The virus uses these to latch onto targets on our cells called ACE2.
Some of the virus variants have developed several mutations in spike which means they don’t get recognised as well by the antibodies we make. This means we are less well protected against some of the new variants. So booster designs are tweaked to make sure they will be better candidates to both boost our waning immunity and broaden the immunity we have to better recognise and tackle variants.
Are annual boosters what we want though?
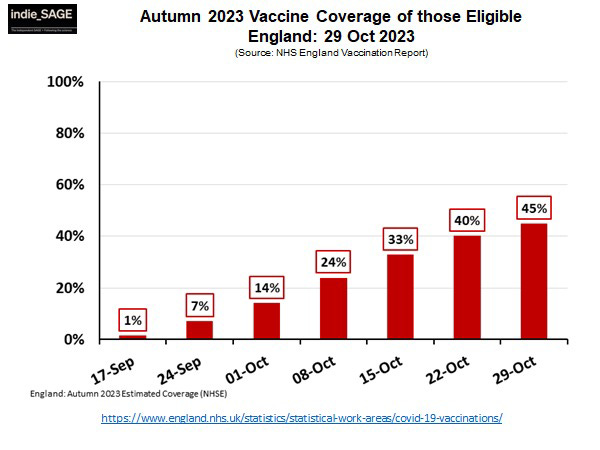
The UK government has so far opted for annual boosters to an ever dwindling pool of eligible recipients. I wrote about my thoughts on this previously so won’t repeat that here. Not only is eligibility narrowing, but vaccine uptake is really dwindling and we are seeing fewer eligible people taking up the vaccines that are being offered (thanks to Kit Yates for image below).
There can be many reasons for this- mixed messages about need, being unsure of eligibility, difficulty accessing clinics and vaccine hesitancy. However, irrespective of the reasons why, its a hugely worrying trend and one that needs to be addressed. Vaccine access across the world is not equal and many countries cannot afford to invest in mRNA booster programmes. mRNA vaccines can also be difficult to store and transport which can limit wider take up.
Other vaccine types do work really well and there has been lots of excitement about Novovax- a protein based vaccine that works very well and is more stable in terms of storage and transport. This vaccine is being used in the USA, approved in the EU but is not, as yet, being used in the UK.
What might happen in the future?
The virus is showing no signs of settling down and a guest on Independent SAGE -Ryan Hisner - beautifully explained how changeable this is and the complexity of tracking it. This means we will still need vaccines but can we think differently.
One approach is to use several features of a virus to develop a so-called multi-variant vaccine. Most current vaccine designs for Covid-19 boosters focus on just spike, but the virus has lots of other features that could be targeted - some of which may be less prone to mutation. This type of approach has been investigated for other diseases including malaria and clinical trials for some multi-variant vaccines have started.
Another approach is dramatically different- it is mucosal vaccination. Conventional needle-in-your-arm vaccines induce a more systemic immune response, mucosal vaccines do something different. Viruses such as SARS-CoV-2 enter our systems via our nose and mouth when we breathe in small virus-containing droplets. This means immunity in our nose, mouth and throat really matters to stop infections.
Mucosal vaccines are designed to target this “mucosal immune system”. The mucosal immune system has the potential to stop the virus in its tracks when it enters the body and prevent infection with the potential for sterilising immunity. Mucosal immunity may also be better at getting our immune system to remember SARS-CoV-2. Systemic vaccines are not so good at activating the memory cells in our nose and throat, but mucosal vaccines are. Mucosal vaccines would probably also be a lot more appealing to those with needle phobias. Some countries like China are already using these vaccines and the US is trialling candidates with promising results.
Vaccine design is only part of the equation!
New types of vaccines are in the pipeline which is exciting to see and I really hope we will see these come through trials and be available soon. Vaccine design is only part of the issue though, we must address the sea of vaccine disinformation that is feeding vaccine hesitancy. We also really need to tackle vaccine equity so that the vaccines are not just available for the wealthiest nations- because - whilst people remain unvaccinated, the virus can continue to thrive and mutate.